Friday, July 25, 2014
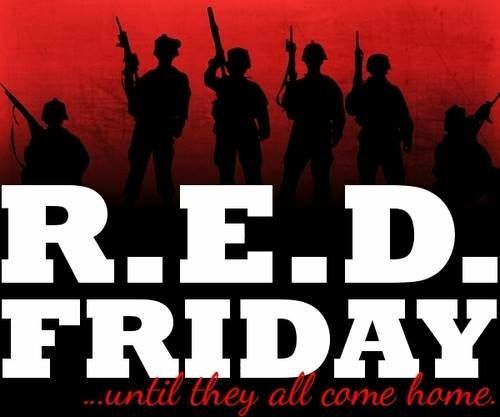
R.E.D. Friday
Today, Veterans stand guard overseas protecting the interests of our Nation in the defense of our freedom. Their sacrifice and service is well deserving of our remembrance. Let us wear red on Friday to show our devotion and support for their service in the name of freedom. May everyone witness this sea of red, and respect our fortitude and unity. May this display provide the morale needed for our soldiers to continue on with their mission, knowing that we await their safe return.
Today, We honor those that never returned with this shining sea of red. With full knowledge of their ultimate sacrifice, we will never forget them. Our act of wearing red is a further example of our dedication to their commitment. This is proof that there are those too that serve those who served the citizens of this Nation at any cost.
Today, Remember Everyone Deployed, Until They All Come Home.
#TYFYS
Veterans PTSD
#veterans #military #milspouse #militaryspouse #REDfriday#remembereveryonedeployed #untiltheyallcomehome #SupportOurTroops#SupportOurMilitary #SupportOurVeterans #Deployed #deployedsoldier#soldier #Army #Navy #AirForce #Marines #NationalGuard #Reserves#NeverForgotten #POWMIA #woundedwarrior #silentsoldier #Vet #Troops#warrior
Tuesday, July 22, 2014
Veteran Suicide and Prevention
22 Veterans commit suicide everyday. 1 is too many, 22 is an injustice and a complete breakdown of our society. There are resources available for our Heroes. If you are a Veteran that needs help, please reach out. The Veterans Crisis Line is a resource available to all, including friends and family. Please, take the first step towards saving a life. Every Veteran is an invaluable part of our way of life, and needs to be preserved at any cost.
People experience emotional and mental health crises in response to a wide range of situations—from difficulties in their personal relationships to the loss of a job. For Veterans, these crises can be heightened by their experiences during military service. When emotional issues reach a crisis point, it’s time to call on the Veterans Crisis Line for support.
Sometimes a crisis may involve thoughts of suicide. Learn to recognize these warning signs:
- Hopelessness, feeling like there’s no way out
- Anxiety, agitation, sleeplessness, or mood swings
- Feeling like there is no reason to live
- Rage or anger
- Engaging in risky activities without thinking
- Increasing alcohol or drug abuse
- Withdrawing from family and friends
The following signs require immediate attention:
- Thinking about hurting or killing yourself
- Looking for ways to kill yourself
- Talking about death, dying, or suicide
- Self-destructive behavior such as drug abuse, weapons, etc.
If you are a Veteran or know a Veteran who is experiencing any of these signs, call the Veterans Crisis Line immediately. Responders are standing by to help.
You can also learn to identify and understand risk factors for suicide.
Identifying the Signs
Many Veterans may not show any signs of intent to harm themselves before doing so, but some actions can be a sign that a Veteran needs help. Veterans in crisis may show behaviors that indicate a risk of harming themselves.
Take a Self-Check Quiz
Crisis, stress, depression, and other issues affect people in different ways. Maybe you’re having trouble sleeping or feel out of control. Maybe your energy level is down or you feel anxious all the time. If these issues and others seem to be leading to a crisis, treatment can help. Take a confidential, anonymous risk assessment to see how you might benefit from VA or community-based services.
You are not alone.
Help is available.
If you are a Veteran in crisis or know one who is, call1-800-273-8255 and Press 1 to confidentially speak with a trained, caring VA responder and get connected to services that can make a difference. Chat online or text with a VA responder to receive anonymous support now. Deaf or hard of hearing individuals using TTY can call1-800-799-4889.
Resource Locator
You can use the resource locator to find VA and community-based support in your area. See how you can connect with VA Suicide Prevention Coordinators, local crisis centers, VA Medical Centers, and more.
If you or a Veteran you know is in crisis, find a facility near you.
Support for Deaf and Hard of Hearing
The Veterans Crisis Line is accessible to individuals who are deaf or hard of hearing. Learn more about support for deaf and hard of hearing individuals.Get Involved and Learn More
Find out how you can support Veterans in crisis. Watch a video about reaching out for help. Learn about resources for homeless Veterans. Or just check out resources VA and other organizations have to offer.
- Spread the Word – download materials for print or web to show support for our Veterans
- Videos – watch encouraging messages of support
- Homeless Resources – learn what support is available for homeless Veterans
- Additional Information – resources for Veterans and their loved ones from VA, military, and civilian communities
- MakeTheConnection.net – connects Veterans and their friends and family members with information, resources, and solutions to issues affecting their health, well-being, and everyday lives. Hear inspiring stories of strength. Learn what has worked for other Veterans. Discover positive steps you can take—all in the words of Veterans just like you.
Veterans PTSD, Inc. asks that everyone that knows of someone at risk of suicide should contact a suicide prevention professional immediately. You can be a hero, just make the call. #TYFYS
Military Sexual Trauma: Disability Compensation
COMPENSATION: MILITARY SEXUAL TRAUMA (MST)
DISABILITY COMPENSATION FOR PERSONAL ASSAULT OR
MILITARY SEXUAL TRAUMA (MST)
Some Veterans may have experienced personal assault or sexual trauma while serving in the military. These kinds of experiences can sometimes affect Veterans’ mental and physical health, even many years later. Veterans can apply for disability compensation for any current difficulties that are related to their service, including difficulties related to personal assault or military sexual trauma (MST). You do not need a VA service-connected disability rating to be eligible for free MST-related treatment through VA. No documentation is required to receive MST-related treatment.
How Does VA Define Personal Assault and Military Sexual Trauma (MST)?
VA defines personal assault as physical or psychological violence, domestic battering, or stalking. One type of personal assault is MST, which is defined by Title 38 U.S. Code 1720D as “psychological trauma…resulting from a physical assault of a sexual nature, battery of a sexual nature, or sexual harassment which occurred while the Veteran was serving on active duty or active duty for training.” Sexual harassment is defined as “repeated, unsolicited verbal or physical contact of a sexual nature which is threatening in character.”
Can You Develop Posttraumatic Stress Disorder (PTSD) or Other Mental Health
Disorders as a Result of Personal Assault or Military Sexual Trauma?
Yes. Exposure to any trauma can potentially result in PTSD or another mental health disorder. PTSD is the most common mental health diagnosis related to experiencing a personal assault or MST.
What Evidence Can Support a Disability Claim for PTSD as a Result of Personal Assault or Military Sexual Trauma?
Department of Defense forms used in reporting incidents of sexual assault or harassment, as well as
investigative reports during military service, are direct evidence to support these claims. However, VA knows
that events involving personal assault or sexual trauma are not always officially reported. Therefore, VA has
relaxed the evidentiary requirements and looks for “markers” (i.e., signs, events, or circumstances) that provide
some indication that the traumatic event happened, such as;
-Records from law enforcement authorities, rape crisis centers, mental health counseling centers, hospitals, or physicians.
-Pregnancy tests or tests for sexually transmitted diseases.
-Statements from family members, roommates, fellow Servicemembers, clergy members, or counselors.
-Request for transfer to another military duty assignment.
-Deterioration in work performance.
-Substance abuse.
-Episodes of depression, panic attacks, or anxiety without an identifiable cause.
-Unexplained economic or social behavioral changes.
-Relationship issues, such as divorce.
-Sexual dysfunction.
How Can You Apply for Disability Compensation?
You can apply for disability compensation by completing VA Form 21-526, Veteran’s Application for Compensation and/or Pension. You may also apply online at http://www.ebenefits.va.gov/ MST specialists and/or Women Veterans Coordinators are available at every VA Regional Office to assist male and female Veterans filing claims related to personal assault or MST. You can find a list of VA Regional Offices by calling 1-800-827-1000 or visiting http://www.va.gov/ For more information about MST-related treatment, visit
www.mentalhealth.va.gov/msthome.asp.
For More Information, Call Toll-Free 1-800-827-1000 or Visit the VA Web Site at http://www.va.gov/
#veterans #military #MST #PTSD #sexualassault #sexualharassment#sexualabuse #rape #depression #anxiety #panicattacks #flashbacks#militarysexualassault #militarysexualtrauma #stopthestigma #helpavet#supportourtroops #militaryspouse #protectourtroops
#TYFYS
Veterans PTSD
Information and Directional Resource Services and Education - Military, Veterans and Supporters
Non-Profit Organization: 794 like this
eBenefits - Homepage
www.ebenefits.va.gov
PTS Fact Sheet- Summary of Veterans Statistics for PTS, Depression and Suicide
PTS Fact Sheet:
Summary of Veterans Statistics for PTS, Depression and Suicide.
- there are over 2.3 million American veterans of the Iraq and Afghanistan wars (compared to 2.6 million Vietnam veterans who fought in Vietnam; there are 8.2 million “Vietnam Era Veterans” (personnel who served anywhere during any time of the Vietnam War)
- at least 20% of Iraq and Afghanistan veterans have PTSD and/or Depression. (460,000 veterans with PTS and Depression)
- 50% of those with PTSD do not seek treatment
- out of the half that seek treatment, only half of them get “minimally adequate” treatment (RAND study)
- 7% of veterans have both post-traumatic stress disorder and traumatic brain injury
- rates of post-traumatic stress are greater for these wars than prior conflicts
- in times of peace, in any given year, about 4% (actually 3.6%) of the general population have PTSD (caused by natural disasters, car accidents, abuse, etc.)
- recent statistical studies show that rates of veteran suicide are much higher than previously thought. The U.S. military acknowledged that suicides hit a record in 2012, outpacing combat deaths. An estimated 22 veterans committed suicide in America each day in 2010, according to a report released Friday by the U.S Department of Veterans Affairs.
- PTSD distribution between services for OND, OIF, and OEF: Army 67% of cases, Air Force 9%, Navy 11%, and Marines 13%. (Congressional Research Service, Sept. 2010)
- recent sample of 600 veterans from Iraq and Afghanistan found: 14% post-traumatic stress disorder; 39% alcohol abuse; 3% drug abuse. Major depression also a problem. “Mental and Physical Health Status and Alcohol and Drug Use Following Return From Deployment to Iraq or Afghanistan.” Susan V. Eisen, PhD
- More active duty personnel died by own hand than combat in 2012 (New York Times).
- The wives, husbands, children, family and friends of the 460,000 recent veterans with PTS and Depression enlarge effects this problem into the millions. Historically, data show that veterans who suffer from PTSD are likely to experience “difficulties maintaining emotional intimacy,” and have a “greatly elevated risk of divorce.” Children of deployed parents, even those as young as three, have been shown to have increased behavioral health problems compared with children without a deployed parent. Deployments may also lead to an increase in the rates of child abuse in military families.
PTS: Simple and Complex
Steve Andreas
The term PTSD is sometimes applied very loosely to any unpleasant memory of an event that continues to trouble someone. Having a deprived childhood, repeated failure in school or business, or being dumped by a lover may be very unpleasant, but it is not usually a life-threatening event. The DSM 5 criteria for PTSD are fairly specific: an exposure to a terrifying life-threatening event, followed by multiple symptoms that persist and don’t resolve over time.
Bill was driving the lead Humvee in a convoy in Iraq when an IED exploded by the roadside, killing several men in the vehicle. Ever since this, Bill has had trouble sleeping because of nightmares reliving the explosion, and frequent daytime flashbacks whenever he hears a loud noise. Since then he has been isolated, drinking too much, feeling depressed, and sometimes exploding into rage.
Bill’s experience satisfies all the DSM 5 criteria for PTSD: The core of PTSD is essentially a phobic response to the terrifying event itself, and can usually be successfully treated using the RTM phobia cure, in which Bill can learn how to view the event as if he were an uninvolved bystander seeing himself going through it from the outside. This is the core of PTSD, and for some sufferers, that’s all there is. The description of John, in chapter 7 ofHeart of the Mind, (pp. 61-63) is an example. One session with the phobia cure resolved all his symptoms.
However, there may be many other aspects that contribute to PTSD, and these are often confused with the core phobic response, even by “experts” in the field. These additional aspects are very different from the core phobic response, and each requires a different intervention to achieve resolution. Some of these are closely associated with the incident itself, while others occur before or after the traumatic event. Let’s explore Bill’s experience further to illustrate these additional aspects.
Aspects closely associated in time. Bill knew that a pop bottle at the side of the road could be a marker for an IED, but he chose to ignore it, so he feels regret for not stopping, and constantly berates himself for his poor judgment, and feels guilty for the deaths that resulted. Bill’s best buddy was killed in the Humvee explosion, and Bill is grieving this loss. In the frenzy of the attack that followed, Bill shot at anything that moved, including two women and several children, and he feels great shame about having caused their deaths.
Aspects that developed afterward. Bill’s legs were severely damaged in the explosion, and had to be amputated, so Bill is also grieving this loss of many different treasured sports and activities. In addition he has TBI, and he is depressed by the formidable task of adapting to these disabilities. He was engaged to a woman with whom he was intensely involved. When she found out about his injuries, she dropped him like a hot rock, and it was as if a part of him died, depriving him of love and support when he needed it most. This is when he started drinking too much, and his rages became worse and more frequent.
Aspects that developed beforehand. Long before Bill joined the army, he suffered repeated verbal (and some physical) abuse from his father, and he internalized this voice, which constantly criticized him no matter what he did. Bill had spent almost a year in the red zone, under constant threat of attack 24/7. The constant anxiety had already made him habitually hypervigilant, sleeping poorly, and reacting instantly to any surprise by becoming fully alert and ready to respond with violence. Bill entered the army as an idealistic gung-ho warrior, but he had already become disillusioned by the gritty reality of war, and had decided that it was a tragic and futile waste, making his burdens utterly meaningless.
Regret, grief, guilt, shame, physical disability, loneliness, insomnia, rages, drug use, self-criticism, depression, generalized anxiety, hypervigilance, violence, disillusion — all of these (and more) may be part of what is often called PTSD. Each of these tends to make the other aspects worse, in a “perfect storm” that often seems to the sufferer to be part of one confusing and tangled ball of chaos and emotional instability. To work successfully with this it is vitally important to be able to separate the different aspects and work with each using different processes that are appropriate.
There are a great many PTSD sufferers, and there is a desperate need for rapid and effective ways of working with them. Most current treatment approaches are simplistic and grossly ineffective. When I asked an Iraq vet I worked with recently about her previous 5 years of treatment, she said:
“I think I saw 8 or 9 different shrinks, and all they wanted to do was give me meds, and then they had all these stupid things they wanted to do, like a tapping thing where you thought about the war and they did this tapping thing, and that was supposed to make it lessen. And they had this finger thing, follow the finger while you thought about the bad — it was stupid! That didn’t do anything; it just kind of pissed me off — and then off to the next shrink. That was a waste of my time… . I like having tools [that I taught her] now because they didn’t give you any of this when we came back… Now I have a way to cope with everything — something to do at least to make it better.”
Frank’s PTS 9-11 Work:
Frank worked in NYC from September 2011 to August 2012. He had responsibility for the psychological rehabilitation of 850 survivors of the AON Corporation all of whom were above the 100th floor of the World Trade Center and 250 of whom had severe PTS symptoms. It was during this time that he realized the effectiveness of the RTM protocol and the need for its’ widespread utilization for traumatized clients.
Nearly a Quarter of New York Veterans Face Mental Health Challenges; More Coordination of Resources Needed, Study Finds
January 26, 2011 (Albany)—Military veterans from New York state who served in Iraq and Afghanistan are at high risk for mental health problems, according to a new study conducted by the RAND Corporation and funded by the New York State Health Foundation.
Nearly a quarter of veterans (22 percent) in New York State were found to have a probable diagnosis of post-traumatic stress disorder and/or major depression. Compared to similar individuals in the general population, the veterans studied were at an eight-fold greater risk of probable PTSD and a two- to four-fold greater risk of major depression.
While many services are available to those in need, more than 40 percent of veterans report being unaware of what help is available or uncertain about how to navigate the systems that provide assistance. Outreach to connect veterans with services and better coordination among government and community agencies is needed, according to the study, which is the first to look at the needs of returning veterans and their families in New York State.
“This study underscores that many returning veterans have mental health needs that require substantial attention from both the Department of Veterans Affairs and other service providers in New York State,” said Terry Schell, the study’s lead author and a senior social scientist at RAND, a nonprofit research organization. “While many services are available, more needs to be done to make sure veterans get the help they need.”
Since October 2001, approximately 2 million U.S. troops have been deployed to Iraq and Afghanistan, and an estimated 85,000 of the troops have returned to New York. Previous national research by RAND has shown that returning veterans are at high risk for mental health disorders and other types of impairments following deployment. (2013 estimates 22,000 PTS affected Veterans in NYS).
“Veterans who have served our country deserve a health system that is easy to understand and easy to access,” said James R. Knickman, president and CEO of the New York State Health Foundation. “This study helps us to understand where there are gaps in services. It should be a priority for the Veterans Administration to improve outreach and coordination of services for all veterans in need.”
The study found that 26 percent of veterans were unsure how to get answers for their questions about treatment. In addition, almost half of the veterans surveyed indicated that they prefer to receive services in the community rather than through the VA system.
In contrast to the high rates of PTSD and depression among veterans, the rate of veterans’ illicit drug use was lower than in the general population, and alcohol misuse was similar to the rate found among comparable individuals in the general population. However, a considerable number of veterans misuse alcohol and might benefit from treatment, according to researchers.
The study also assessed the needs of veterans’ spouses. Spouses reported experiencing several challenges after their veterans return from deployment. Nearly half reported problems dealing with their veteran spouse’s mood changes and 42 percent were worried about the possibility of future military deployments.
RAND researchers say one clear finding from the study is that veterans’ health and well-being are the responsibility of more than just the Department of Veterans Affairs. Veterans are frequently using providers from government-run programs other than the VA and from the civilian health care system.
“The needs of veterans are not addressed solely through the VA,” said study co-authorTerri Tanielian, co-director of the RAND Center for Military Health Policy Research. “Veterans need services that may be better accessed through private providers, non-profit organizations or public health programs. These different systems must work together with the VA to provide veterans access to high-quality, coordinated care.”
Researchers recommend more effort be put into connecting veterans with care coordinators who can provide personalized assistance across a range of service sectors. The existing system often misses the veterans most in need of outreach — those who have not yet enrolled in the Veterans Health Administration.
The study focused on people living in New York state who deployed overseas, then returned to the community. Unlike most other studies of veterans, RAND researchers drew from all veterans across the state, not just those receiving services from the Department of Veterans Affairs.
Researchers surveyed 913 veterans and 293 spouses of veterans from New York, and conducted six focus groups of veterans and their family members across the state. In addition, they documented services for veterans that are currently available in New York state.
The report, “A Needs Assessment of New York State Veterans: Final Report to the New York State Health Foundation,” can be found at www.rand.org. The study is part of the New York State Health Foundation’s Initiative for Returning Veterans and Their Families, which aims to advance solutions to address the needs of Iraq and Afghanistan veterans and their families.
RAND Health, a division of the RAND Corporation, is the nation’s largest independent health policy research program, with a broad research portfolio that focuses on quality, costs and health services delivery, among other topics.
The RAND Corporation is a nonprofit institution that helps improve policy and decisionmaking through research and analysis. To sign up for RAND e-mail alerts:http://www.rand.org/newsletters.html. RAND is a registered trademark
The New York State Health Foundation is a private Foundation dedicated to improving the health of all New Yorkers. NYSHealth has a three-part mission: expanding health insurance coverage, increasing access to high-quality health care services, and improving public and community health by educating New Yorkers about health issues and empowering communities to address them. It was established with charitable funds from the privatization of Empire Blue Cross/Blue Shield.
New York State Health Foundation 1385 Broadway, 23rd Floor | New York, NY 10018 | 212-664-7656
Moral guilt:
- The “elephant in the room” with recent veterans mental problems is the lack of meaning in the recent “discretionary wars” and the effect wars hell has on individuals who do not believe in the underlying purpose of the conflict. See the articles below.
The true Author/Authors of this are not known by Veterans PTSD. This article was found on a Facebook Page: The Research and Recognition Project-The Road Back. We did, however, find the results interesting. We do not endorse, nor support, the findings without knowledge of their legitimacy. We do believe the that the authors intentions are on the right-side of the topic. Please take what you wish from this, and leave the rest behind. #TYFYS
OPERATION: BOOTS TO BUSINESS
Boots to Business builds on SBA’s role as a national leader in entrepreneurship training. Leveraging our ongoing collaboration with Syracuse University’s Institute for Veterans and Military Families (IVMF), SBA delivers Boots to Business with the support of its field offices and Resource Partners, such as the Small Business Development Centers (SBDCs), Women’s Business Centers (WBCs), SCORE, and Veterans Business Outreach Centers (VBOCs). SBA’s expert Resource Partner network already provides entrepreneurship training to more than 100,000 veterans every year, many of whom are service members transitioning out of the military.
OPERATION: BOOTS TO BUSINESS http://boots2business.org/default.aspx
Transitioning Veterans Fly Free for Job Interviews
Hire Our Heroes (HOH) in partnership with Armed Forces Foundation (AFF) will provide a free, round-trip ticket to any transitioning veteran going on a job interview anywhere in the country.
If you are currently actively engaged in the final steps of a job interview out of state, where the final step is that you fly in for a face to face interview, HOH will fly you there for free.
HOH will provide a free round trip airline ticket to any transitioning veteran interviewing to secure a job without the means to travel to and from the interview. The idea here is to support small to medium size businesses by allowing them to tap into an untapped market of talent that they might not typically have access to, due to budget constraints. In addition, this allows transitioning veterans the opportunity to interview and secure opportunities prior to making the final transition back into the civilian world.
HOH hopes that by providing these benefits to all transitioning veterans, the odds of securing employment are greatly increased.
Transitioning Veterans Fly Free for Job Interviews -FAQ:
Q: Who is eligible
A: This program is targeted towards all transiting service members who have recently separated from the service within the last year or plan to separate within the next 90 days.
A: This program is targeted towards all transiting service members who have recently separated from the service within the last year or plan to separate within the next 90 days.
Q: How much does this cost
A: There is no charge for veterans or the hiring entity
A: There is no charge for veterans or the hiring entity
Q: What is required in order to qualify for the free travel
A: The ticket will be provided to any veteran that is in the final stages of an interview for employment. A face to face interview and or a Skype interview should have been conducted up until this point. HOH will require the hiring company’s details in order to verify the interview process and where you stand as it pertains to the opportunity and their hiring process.
A: The ticket will be provided to any veteran that is in the final stages of an interview for employment. A face to face interview and or a Skype interview should have been conducted up until this point. HOH will require the hiring company’s details in order to verify the interview process and where you stand as it pertains to the opportunity and their hiring process.
Q: How do I get the ticket
A: First steps is to validate your credentials through Troop ID. Once your credentials have been validated you will receive a follow up email on next steps. HOH will book the ticket for you and provide you with a paper ticket at the time of travel.
A: First steps is to validate your credentials through Troop ID. Once your credentials have been validated you will receive a follow up email on next steps. HOH will book the ticket for you and provide you with a paper ticket at the time of travel.
Q: If I have already separated over a year ago am I still eligible?
A: Yes, although directed towards the immediate transitioning veterans, all veterans will receive the same opportunity.
A: Yes, although directed towards the immediate transitioning veterans, all veterans will receive the same opportunity.
Q: How many tickets are there
A: There are a limited number of tickets available and the offer is on a first come first serve basis. Tickets are for immediate travel, have no cash value, cannot be sold and are non-transferable.
A: There are a limited number of tickets available and the offer is on a first come first serve basis. Tickets are for immediate travel, have no cash value, cannot be sold and are non-transferable.
Q: Do I still qualify for this benefit if I’m working with a staffing company, a.k.a. A headhunter?
A: Unfortunately we do not offer this benefit if you are working with a staffing company or will be attending a job fair they might be putting on.
A: Unfortunately we do not offer this benefit if you are working with a staffing company or will be attending a job fair they might be putting on.
Q: What airline will I be flying on
A: The tickets are for Southwest airlines. Travel is only available anywhere that Southwest fly’s to and from.
A: The tickets are for Southwest airlines. Travel is only available anywhere that Southwest fly’s to and from.
PTSD and Problems with Alcohol Use
PTSD and alcohol use problems are often found together. This pairing can be big trouble for the trauma survivor and his or her family.
People with PTSD are more likely than others with the same sort of background to have drinking problems. By the same token, people with drinking problems often have PTSD. Those with PTSD have more problems with alcohol both before and after getting PTSD. Having PTSD increases the risk that you will develop a drinking problem.
Women who go through trauma have more risk for drinking problems. They are at risk for drinking problems even if they do not have PTSD. Women with drinking problems are more likely than other women to have been sexually abused at some time in their lives. Both men and women who have been sexually abused have higher rates of alcohol and drug use problems than others.
Up to three quarters of those who have survived abusive or violent trauma report drinking problems. Up to a third of those who survive traumatic accidents, illness, or disasters report drinking problems. Alcohol problems are more common for survivors who have ongoing health problems or pain.
Sixty to eighty percent of Vietnam Veterans seeking PTSD treatment have alcohol use problems. War Veterans with PTSD and alcohol problems tend to be binge drinkers. Binges may be in response to memories of trauma. Veterans over the age of 65 with PTSD are at higher risk for a suicide attempt if they also have drinking problems or depression.
If you have a drinking problem, you are more likely than others with your same sort of background to go through a psychological trauma. You may also have problems getting close to others. You may have more conflicts with those people to whom you are close.
Problems with alcohol are linked to a confused and disorderly life. This kind of life leads to less closeness and more conflict within a family. The confusion of a life with a drinking problem makes it harder to be a good parent.
You may drink because using alcohol can distract you from your problems for a short time. You should know, though, that drinking makes it harder to concentrate, be productive, and enjoy all parts of your life.
Using too much alcohol makes it harder to cope with stress and your trauma memories. Alcohol use and intoxication (getting drunk) can increase some PTSD symptoms. Examples of symptoms that can get worse are numbing of your feelings, being cut off from others, anger and irritability, depression, and the feeling of being on guard.
If you have PTSD, you may have trouble falling asleep or problems with waking up during the night. You may “medicate” yourself with alcohol because you think it’s helping your sleep. In fact, using too much alcohol can get in the way of restful sleep. Alcohol changes the quality of your sleep and makes it less refreshing.
If you have PTSD, you may have bad dreams or nightmares. You may drink because you think using alcohol will decrease the number of bad dreams or how scary they are. Yet drinking just continues the cycle of avoidance found in PTSD. Avoiding the bad memories and dreams actually prolongs the PTSD. You cannot make as much progress in treatment if you avoid your problems. Alcohol use problems make PTSD treatment less effective.
When you suddenly stop drinking, the nightmares often get worse. Working with your doctor on the best way to reduce or stop your drinking makes cutting back on alcohol easier. You will be more likely to have success in your efforts.
If you have both PTSD and drinking problems, you are likely to have other mental or physical health problems. Up to half of adults with both PTSD and drinking problems also have one or more of the following serious problems:
- Panic attacks, extreme fears or worries, or compulsions (being driven to do things like checking the door locks over and over)
- Mood problems such as depression
- Attention problems or behaving in ways that harm others
- Addiction to or abuse of street or prescription drugs
- Long-term physical illness such as diabetes, heart disease, or liver disease
- Ongoing physical pain Having both PTSD and a drinking problem can make both problems worse. For this reason, alcohol use problems often must be part of the PTSD treatment. If you have PTSD, plus you have, or have had, a problem with alcohol, try to find a therapist who has experience treating both issues.In any PTSD treatment, several points related to alcohol should be stressed:
- When planning your treatment, you should discuss with your therapist the possible effects of drinking on your PTSD symptoms. As noted above, alcohol can affect sleep, anger and irritability, anxiety, depression, and work or relationship problems.
- Treatment should include education, therapy, and support groups that help you with your drinking problems in a way you can accept.
- Treatment for PTSD and alcohol use problems should be planned in a way that gets at both problems together. You may have to go to separate meetings on each issue, or see providers who work mostly with PTSD or mostly with alcohol problems. In general, though, PTSD issues should be included in alcohol treatment, and alcohol use issues should be included in PTSD treatment.
- Once you become sober (stop drinking entirely), you must learn to cope with your PTSD symptoms in order to prevent relapse (return to drinking). This is important because sometimes the PTSD symptoms seem to get worse or you notice them more right after you stop drinking. Remember that after you have stopped drinking, you have a better chance of making progress in your PTSD treatment. In the long run, you are more likely to have success with both problems.
Subscribe to:
Comments (Atom)